Navigating Miscarriage: The Toll on Women's Health and Pathways to Healing with Partner Support
Discover how miscarriage affects women's mental and physical health, with peer-reviewed insights. Learn recovery strategies like mindfulness and nutrition, plus how spouses can support healing through empathy and shared rituals.
Miscarriage, the spontaneous loss of a pregnancy before 20 weeks, is a heartbreaking experience that affects millions of women worldwide each year. With estimates suggesting it occurs in 10-20% of known pregnancies, it's far more common than many realize, yet it remains shrouded in silence and stigma. This not only isolates those affected but also hinders open discussions about its profound impacts on mental and physical health. Beyond the immediate grief, miscarriage can trigger a cascade of emotional and bodily challenges that linger, influencing future pregnancies, relationships, and overall well-being. Fortunately, recovery is possible through self-care, professional support, and the involvement of partners. Drawing from research, this article explores these effects in depth, offers guidance for women on reclaiming their health, and highlights how spouses can provide meaningful assistance. By fostering understanding and action, we aim to empower those navigating this loss toward resilience and hope.
The Mental Health Effects of Miscarriage
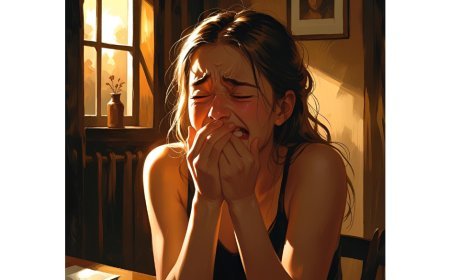
The emotional aftermath of miscarriage is often intense and multifaceted, encompassing grief, anxiety, depression, and even trauma that can disrupt daily life. Women may grapple with profound sadness over the lost potential of life, compounded by feelings of guilt, shame, or failure—emotions that stem from societal expectations around motherhood and the internalized belief that they "should have" prevented the loss. In the short term, this can manifest as acute distress: insomnia, loss of appetite, irritability, or withdrawal from social interactions. Studies indicate that up to 55% of women exhibit depressive symptoms immediately following a spontaneous abortion, while more than 18% report moderate anxiety levels. These reactions are not mere sadness but can meet clinical criteria for disorders like major depression or post-traumatic stress, particularly if the miscarriage involved medical interventions or was recurrent.
Long-term effects are equally concerning, with symptoms persisting for months or years if unaddressed. For instance, recurrent miscarriages—affecting 2-6% of couples—affect mental health deeply, with around 10% of women showing moderate to severe depression and over 40% experiencing high stress. This prolonged state can lead to avoidance behaviors, such as fearing future pregnancies, which heightens isolation and strains relationships. Cultural factors play a role too; in some societies, blame is placed on the woman, exacerbating shame and leading to social withdrawal. Research also shows that Black women may be twice as likely to develop major depression post-loss compared to non-Black women, highlighting disparities influenced by socioeconomic status and access to care. Moreover, the hospital environment during miscarriage can intensify these effects—insensitive terminology like "termination" or lack of privacy in emergency departments often leaves women feeling dismissed, with 28.71% reporting insufficient psychological support from physicians and 22.44% receiving none at all. Men, too, face emotional turmoil, though it's frequently overlooked; they report grief and isolation, feeling excluded from care that focuses solely on the woman, which can indirectly worsen the couple's shared mental health burden. Overall, these mental health impacts underscore the need for compassionate, timely interventions to prevent chronic issues like lowered self-esteem or relational discord.
The Physical Health Effects of Miscarriage
While the emotional scars of miscarriage are widely acknowledged, its physical repercussions are equally significant, often intertwining with mental health to create a holistic challenge. Immediately after a miscarriage, women may endure cramping, heavy bleeding, and fatigue as the body expels tissue, with risks of infection or incomplete evacuation requiring medical procedures like dilation and curettage. These symptoms can last weeks, disrupting work, exercise, and intimacy, and leaving women feeling vulnerable or out of control. Hormonal fluctuations post-loss mimic postpartum changes, leading to mood swings, breast tenderness, or irregular cycles that persist for months, further taxing the body.
In the longer term, miscarriage can signal underlying health issues, such as hormonal imbalances or uterine abnormalities, increasing risks for future complications like preterm birth or low birth weight in subsequent pregnancies. Research links pregnancy loss to heightened physical exhaustion and pain; for example, women who've experienced stillbirth (a related late loss) report more frequent physical complaints and lower quality of life even a decade later, with effects like chronic fatigue not diminishing over time. Recurrent miscarriages amplify this, correlating with elevated stress that contributes to adverse outcomes like hypertension or gestational diabetes in future gestations. The interplay with mental health is evident: depression and anxiety can manifest somatically as headaches, gastrointestinal issues, or weakened immunity, while physical recovery delays—like persistent bleeding—can exacerbate emotional distress, creating a vicious cycle. Factors like low socioeconomic status or prior childlessness heighten these risks, as do inadequate medical follow-up, which leaves women without guidance on resuming activities or monitoring for complications. Addressing physical health promptly is crucial, as unresolved issues can erode overall vitality and complicate healing.
Recovery Strategies for Women: Mental and Physical Healing
Recovering from miscarriage requires a compassionate, multifaceted approach that honors both mind and body, allowing women to process grief while rebuilding strength. Mentally, acknowledging the loss is foundational; women benefit from validating their emotions through journaling, therapy, or support groups, which help mitigate isolation. Cognitive-behavioral techniques can reframe guilt, while mindfulness practices like meditation reduce anxiety by grounding in the present. Protective factors include strong social networks, higher education, and satisfaction with healthcare—women who receive empathetic care report better coping. For recurrent losses, "tender loving care" approaches, involving emotional support and monitoring, have shown success rates of 86% in subsequent pregnancies versus 33% without. Physically, rest is paramount in the initial weeks, with gentle activities like walking aiding circulation and mood. Nutrient-rich diets support hormonal balance—focusing on iron for blood loss and omega-3s for inflammation—while avoiding alcohol or caffeine prevents further disruption. Regular check-ups ensure complete recovery, and tracking cycles via apps can empower women planning future conceptions.
Hospital experiences influence recovery; positive interactions, such as clear information on causes and options, alleviate distress, while interventions like bereavement protocols or web-based counseling have reduced grief and anxiety in follow-ups. Women often desire written resources on emotional journeys and future risks, as verbal information is hard to retain amid shock. Culturally sensitive memorials, like remembrance services, aid closure. Overall, gradual integration of self-care routines fosters resilience, with professional help sought if symptoms like persistent sadness linger beyond a few months.
How Spouses Can Provide Support
Spouses play a pivotal role in miscarriage recovery, offering emotional anchorage that eases isolation for both partners. Men often grieve silently, feeling sidelined by healthcare focused on women, yet their involvement strengthens mutual healing. Key is open communication: spouses should listen without minimizing the loss, using phrases like "I'm here with you" to validate feelings. Practical support, such as handling household tasks or attending follow-ups, lightens the load, while encouraging shared rituals—like planting a memorial tree—fosters connection. Research shows men benefit from recognition too; acknowledging their grief prevents resentment, with 66.3% at risk for anxiety post-loss. In hospitals, spouses appreciate inclusion—clear information helps them support effectively, reducing their sense of helplessness. For LGBTQ partners, tailored validation is vital. Long-term, couples therapy addresses relational strains, promoting empathy and intimacy recovery.
Here are the details of three key peer-reviewed articles referenced:
- Title: Pregnancy loss: Consequences for mental health
Authors: Diana Cuenca
Journal Name: Frontiers in Global Women's Health
Publication Date: January 23, 2023 - Title: Factors affecting the emotional wellbeing of women and men who experience miscarriage in hospital settings: a scoping review
Authors: Martina Galeotti, Gary Mitchell, Mark Tomlinson, Áine Aventin
Journal Name: BMC Pregnancy and Childbirth
Publication Date: March 31, 2022 - Title: Toward Optimal Emotional Care During the Experience of Miscarriage: An Integrative Review of the Perspectives of Women, Partners, and Health Care Providers
Authors: Lysha Lee, Winn Ma, Sidney Davies, Marjolein Kammers
Journal Name: Journal of Midwifery & Women's Health
Publication Date: November 12, 2022
Actionable Steps for Recovery
- For Mental Health Recovery: Journal daily about your feelings to process grief; seek therapy or a support group within the first month; practice 10 minutes of mindfulness meditation each day to ease anxiety.
- For Physical Health Recovery: Rest for at least a week post-miscarriage, incorporating gentle walks; eat iron-rich foods like spinach and lean meats to rebuild strength; schedule a follow-up doctor's visit two weeks after to monitor healing.
- For Spouses to Help: Listen actively without offering fixes, validating emotions weekly; share household duties to allow rest; attend a joint counseling session to discuss shared grief and strengthen your bond.
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0