The Hidden Link: Lyme Disease and Mental Health Symptoms
Discover the Lyme-mental health link: Brain fog & fatigue causes. Learn neurofeedback, molybdenum & more to help! Read now!

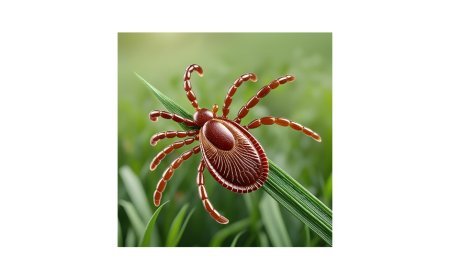
Lyme disease, a tick-borne illness caused by the bacterium Borrelia burgdorferi, is often recognized for its physical symptoms like joint pain and fatigue. However, its impact on mental health is less understood, yet equally profound. Symptoms such as brain fog, anxiety, depression, and fatigue can overlap with mental health conditions, creating a diagnostic challenge for families. Experts like Dr. Kendra Becker, Jennifer Giustra, Beth Lambert, Maria Rickert Hong, and Dr. Roseann Capanna-Hodge have shed light on this connection, emphasizing that Lyme can mimic or exacerbate psychiatric issues. This article explores why Lyme triggers these symptoms, offers practical strategies—including vitamins like molybdenum, chiropractic care, and probiotics—to manage brain fog and fatigue, and provides resources to support affected families.
Why Lyme Causes Mental Health Symptoms
Lyme disease can penetrate the blood-brain barrier, leading to inflammation in the central nervous system—a condition known as neuroborreliosis. This inflammation disrupts normal brain function, affecting areas responsible for mood, cognition, and energy regulation. The bacterium’s outer surface proteins trigger immune responses that cause “itis” conditions—meningitis, encephalitis—resulting in symptoms like brain fog, memory issues, and personality changes. Chronic untreated cases may lead to neurotransmitter imbalances, contributing to anxiety, depression, or even rare instances of psychosis. Fatigue arises from the body’s ongoing battle with the infection, compounded by poor sleep and stress, which further tax mental resilience. Experts suggest this overlap often leads to misdiagnosis as primary psychiatric disorders, delaying proper treatment and leaving families in distress.
Overlapping Symptoms: Lyme and Mental Health
The mental health symptoms of Lyme mirror conditions like ADHD, anxiety, and depression. Brain fog—described as slowed processing or confusion—impairs focus and memory, resembling executive dysfunction. Anxiety and irritability affect 40% of those with disseminated Lyme, while fatigue can trigger sleep disturbances, amplifying mood swings. These symptoms can persist post-treatment in 10-20% of cases, a phenomenon sometimes called post-treatment Lyme disease syndrome (PTLDS), though its mechanisms remain debated. This overlap complicates diagnosis, as traditional psychiatric labels may overlook the infectious root, a point raised by advocates like Beth Lambert and Maria Rickert Hong, who highlight the need for comprehensive medical evaluations.
Managing Brain Fog and Supporting Families with Fatigue
Addressing these symptoms requires a multifaceted approach, blending lifestyle adjustments with professional support. Here are expanded strategies, including new additions:
-
For Brain Fog: Cognitive exercises like puzzles or memory games can stimulate mental clarity. Dr. Roseann Capanna-Hodge advocates neurofeedback, a non-invasive technique that trains the brain to regulate activity, reducing brain fog by calming overactive neural patterns. Simple routines, like breaking tasks into 10-minute segments with breaks, also help maintain focus. Add molybdenum (200-500 mcg daily), a trace mineral that supports detoxification and reduces brain fog by aiding sulfur metabolism, under medical supervision. Chiropractic adjustments can improve nervous system function, potentially clearing cognitive haze by aligning the spine and reducing inflammation.
-
For Fatigue: Encourage gentle movement, such as 15-minute walks, to boost energy without exhaustion. Families can create a rest schedule with short naps (20-30 minutes) to combat daytime lethargy, a strategy Jennifer Giustra emphasizes for restoring balance. Prioritizing hydration and nutrient-dense foods (e.g., leafy greens, nuts) supports energy levels. Incorporate probiotics (e.g., 10-20 billion CFU daily of Lactobacillus or Bifidobacterium strains) to enhance gut health, which influences energy and mood via the gut-brain axis, a tactic supported by integrative health experts.
-
Family Navigation: Open communication is key. Parents should track symptoms and moods in a journal to identify patterns, aiding discussions with healthcare providers. Involving siblings in light, supportive tasks—like preparing a snack together—can reduce the caregiving burden and foster a team spirit, a tactic supported by Beth Lambert’s family-centered approaches.
Resources for Families
Navigating Lyme’s mental health impact can feel isolating, but resources abound:
-
Project Lyme (projectlyme.org): Offers educational materials on mental health symptoms and self-assessment tools, reflecting insights from experts like Dr. Kendra Becker.
-
Zen Psychological Center (zenpsychologicalcenter.com): Provides compassionate support and practitioner listings, including integrative options inspired by Maria Rickert Hong’s work.
-
Dr. Roseann Capanna-Hodge’s Website (drroseann.com): Features neurofeedback guidance and holistic strategies, aligning with her expertise in Lyme-related mental health.
These resources empower families to seek validated care and connect with others facing similar challenges.
A Path to Healing
Lyme disease’s mental health symptoms stem from its neurological and inflammatory effects, often misunderstood as purely psychiatric. By addressing brain fog with cognitive tools, neurofeedback, molybdenum, and chiropractic care, and managing fatigue with rest, exercise, probiotics, and family support, families can reclaim stability. The insights from Becker, Giustra, Lambert, Hong, and Capanna-Hodge underscore the importance of looking beyond conventional diagnoses. With the right resources and a proactive approach, families can navigate this complex illness with hope and resilience.
***This article is for informational purposes only and does not constitute medical advice. The content is not intended to diagnose, treat, cure, or prevent any disease or medical condition. Always consult a licensed physician or healthcare professional before making any decisions regarding your health, including genetic testing, dietary changes, or treatment options related to ADHD or any other condition.
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0